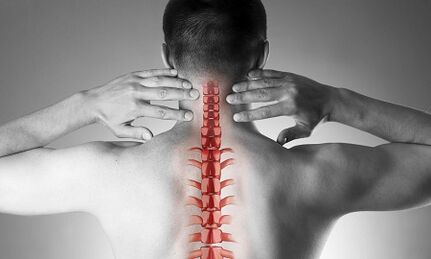
Cervical osteochondosis, or spondylosis, occurs as a result of changes in the form and structure of the vertebrae.Despite the fact that the cervical region is short enough compared to the total length of the spine, it may be the most important part of the spine.Each pair of neighboring vertebrae forms the intervertebral holes through which the nerve roots go and go to each muscle and organ of the upper half of the body.Through other holes - in the lateral processes of these vertebrae - the vital vessels provide blood supply to the brain.
The causes of osteochondrosis of the cervical column
The causes of osteochondrosis are:
- injuries,
- "Sedentary" work in the instructor located under the level of the eyes,
- physical work associated with weight transfer,
- Long -term stay to drive a car,
- Work "on the phone" without using distance peripherals (in this case, the operator presses the phone to the shoulder of the ear)
- Constitutional characteristics (hot and congenital changes in cervical vertebrae, short neck)
Formation of pathological vertebral changes
With osteochondrosis, small points are starting to form on the edges of vertebral bodies, which can hurt the nearby structures.Most often, this happens in response to an excessive charge on the cervical compartment, and not only the result of the "aging" of the intervertebral joints (remember that it was used to be considered as degenerative osteochondosis, then natural "age-related" disease, such as osteoarthrosis).As the disease develops, the closing plates of the vertebrae and a decrease in the height of the intervertebral discs occur.These discs are normal play the role of the shock absorber between the vertebrae and, among other things, prevent damage to the vertebral roots.With progressive osteochondosis, a (hernia) in protruding (hernia) of the core of the intervertebral disc jacket occurs, on which during the disease, there is more and more pressure while weakening the "restraint" of the ligaments on all sides.This hernia is also able to tighten vertebral structures and cause neurological manifestations of the disease.
What are the symptoms of cervical osteochondosis?
Osteochondrosis of the cervical column with pain syndrome
All pain in the neck forces the pathology of the cervical column.In terms of growth, the intensity of pain syndrome is divided into 4 stages, the first patient feels numbness, tingling, a feeling of "waterproofing" in the field of a certain muscle group, in the fourth stage - the most serious - the pain is so intense that it leads to the immobility of the patient and the loss of performance.
In addition to pain syndrome in the cervical and occipital region, the patient notes "reflected" (radiant) pain in the upper limb, the side areas of the chest sub-service.
Osteochondrosis of the cervical column with root syndrome
They speak of involvement in the process of nerve roots when pain, numbness and tingling spread to the lower jaw, upper back, forearm and fingers.At the same time, the patient draws attention to the fact that he "seemed to leave" his hand, he was very practically sleeping.Morning stiffness in the finger joints, does not last more than 10 to 15 minutes, is noted.With the development of radicular syndromes, during examination, a decrease in muscle strength of the upper limbs can be noted.
Osteochondrosis of the cervical column with the "vertebral artery syndrome"
Regarding the involvement in the process of the blood vessels (pressing them with an hernial projection or an osteophyte), they say that when the patient complains of frequent attacks of headache, especially after a long stay in a certain position, when he is thrown from the head (for example, during swimming with a milk this clinical situation is well detected using ultrasound (with the "Doppler "). With ultrasound, the inquisition of vertebral arteries, the narrowing of their light is determined. In this case, we can speak of surgery, because a pronounced change in blood circulation in the vertebral arteries is a risk factor for the development of stroke.
Osteochondrosis of the cervical column with "heart syndrome (heart)"
This syndrome obliges the patient to mainly contact the cardiologist, because the main complaints concern pain in the left half of the chest, the sub-scapular region, which weakens or intensifies when physical activity is carried out or body position.After the exclusion of myocardial infarction and other heart disease, the patient is observing and the treatment of a neurologist and an orthopedist.
Diagnosis
To clarify the diagnosis, four methods are used: radiography, ultrasound, computed tomography and magnetic resonance imaging.
The most affordable method is always the radiography of the cervical column, the most informative is the radiography of the lateral projection ("lateral view").This method allows in the first approximation to establish the presence of an injury, raw structural changes in the vertebrae.
The ultrasound examination (ultrasound) is carried out to clarify the state of the vertebral arteries.With the help of this method, they discover if the blood flow is disturbed, and if so, to what extent and what type of obstacle has appeared and where they are located.
Tomodensitometry (CT).It allows you to more precisely assess the state of bone structures, the degree of bone density, allows you to see smaller osteophytes (bone growths) as possible with the X -ray.
Magnetic resonance imaging (MRI).This type of examination is essential for the suspected hernias, the precise location of the spinal cord damage and the degree of these damage.This study is necessary if the question is raised from surgical (surgical) treatment of cervical column disease.
Treatment of cervical osteochondosis
Drugs
The standard set of products for the treatment of cervical osteochondosis reflects the purpose of treatment: relieving pain syndrome, eliminating painful muscle spasms and inflammation of nerve roots, increasing the mobility of the spine.To achieve these objectives, mainly the use of pain relievers, NSAIDs - non -steroidal anti -inflammatory drugs, muscle relaxants are used.It should be remembered that the self-medication of these groups can be dangerous, because there is a possibility of erroneous interpretation of the symptoms, as well as the underestimation of the side effects of these drugs.Local drugs (Basel) among NSAIDs in the form of gels are widely used, and if the pain is stopped, the same drugs can already be used in the form of ointments.
For the treatment of osteochondrosis at a deeper and basic level, systemic drugs are used.These substances restore the structures of the cartilage of the vertebrae, prevent their additional damage.The treatment courses are long, the effect persists for several months.
Cervical osteochondosis has significant differences in relation to the pathology of the spine.The pain in the neck in this case may not be caused by signals of the nerves of the suffering spine, but by painful chronic muscle surmount - everything together is called muscle - tonic syndrome.It is a completely "benign" state, which is well treated with the same set of drugs: non-steroidal anti-inflammatory drugs, muscle relaxing, using an intramuscular "blockage" using steroids.Usually the doctor reveals acute pain during his survey of the "trigger" points of So-appels along the whole cervical column, as well as in the muscles of the upper shoulder belt.More often, such a pathology occurs in women, mainly under 40 years of age.Despite the pronounced pain syndrome, the vascular nore structures remain intact, the blood flow in the head of the head does not suffer.
Manual therapy
This treatment method can be effective for recently occurred pain (often following a small injury, subluxation) in the neck, not accompanied by dizziness, other changes in the nervous system and the circulatory system.It is allowed to use manual therapy only after an in -depth examination, in addition, the doctor carrying out this procedure should have sufficient experience in the field of trauma and orthopedics.With "old" forms of disease, the use of manual therapy is dangerous!
Two methods of this type of intervention are known:
- manipulation (short influences of a significant force aimed at eliminating subluxation, well -known "bone clicks");
- Mobilization (the method is based on a smooth neck stretching after warming up and relaxing the muscular corset of the neck).
A combined method based on a combination of two main ones is also used.It is important to remember that in addition to these contraindications, manual therapy is prohibited for any disease, accompanied by an increase in blood pressure, for any pathology of the thyroid and ent or ent-organe gland.
Treatment of cervical osteochondrosis at home
Medical gymnastics for cervical osteochondosis
The first and main rule for beginners to engage in physiotherapy exercises is not to perform exercises, overcoming painful sensations.Of course, you should not start in the "acute" period when the pain has just appeared.Another important recommendation is to avoid sudden movements and circular movements in the cervical region.
Each lesson must start with a short light self-massage of the neck muscles.
The following is a warm-up "warming":
- The hands are lowered along the body, the shoulders are equal, the back is straight (you can check the posture by slightly pressed with heels, shoulder blades and buttocks to the wall).We walk instead of 1 min on the whole foot, 1 min - on socks, 1 min - on the heels.
- The starting position is the same.We tighten the brushes in the fists, putting on the shoulders, our hands are straightened.The movements are slow, we make 20 repetitions, the last climb is greater than 5 seconds.We make sure that the neck muscles are not "tight".
- The starting position is the same.We include our heads in turn in the right, then on the left side.The movements are smooth, a slope on 8 accounts, at the extreme point of inclination - maintain 8 seconds.
- The starting position is the same or seated on a hard chair.Smooth head inclinations from the head to the extreme - maintain 8 seconds
- The starting position is the same or seated on a hard chair.Slowly include the head forward, until the chin in the chest, then slowly turns the head to the right (with 4 accounts) and to the left (with 4 accounts).Do not allow muscle tension.
- The starting position is the same or seated on a hard chair.We raise your shoulders on 4 accounts, then we also lower them in 4 counts.10 repetitions.
- The starting position is the same or seated on a hard chair.We raise our shoulders, but now we make circular movements at the front at the rear, 8 accounts.10 repetitions.
- We align the back, check the posture.For 4 accounts, we reduce the shoulder blades behind your back, trying to connect them, at the end point, we linger for 8 seconds, then we return to the starting position.
Pillows
As already mentioned, hypertonicity of neck muscles is the first and often the main reason for the development of cervical osteochondosis.A rational selection of pillows and mattresses, guaranteeing a relaxed and comfortable position during sleep is no less than gymnastics, physiociette and drugs.
When you choose a mattress, pay attention to the composition of the filling (the products are suitable, at least half in coconut chips, that is to say with a sufficient degree of rigidity).The soft spring mattresses do not allow the spine sufficiently enough.The most optimal sleep for sleep is on the side, pull one or the two knees in the stomach.The pillow should be located so as to fill the entire space between the shoulder, the ear and the matrate, the parietal part (crown) of the head is on the same horizontal line with the spine.To avoid too high and too low, as well as soft pillows.The ideal option is the product of an ergonomic shape, that is to say in this case, with a small compression of compression on one side.
General recommendations
Pay attention to the posture.During the walk or in a standing, the position is a position when the chest comes out forward and the stomach is fired.
Avoid long -term stay in a seated position.A simple rule of prevention of cervical osteochondosis is known: after 60 minutes of work, a period of walking or warm -up of 10 to 15 minutes is necessary.
A work chair should have a high headrest or a back.
In a sitting position, the legs must rest on the ground and the neck should not be tense.To this end, use special orthopedic devices: rollers under the neck when you drive in a car, a pillow under your back.
Avoid weight lifting.If necessary, kneel, press the heavy object to the body, then keep yourself gently using the strength of the leg muscles, but not the "push" of the back.
Do not lean with the straightened legs.Use supports, work surfaces in order to bring the object closer to yourself and not persuade your face about it.Try to do your homework sitting in a chair or a gymnastics ball.
If you need to use a mop, a broom or a rake, do not wipe your arms, back and neck, do not lean on the side.
Avoid swimming in the style of brass.























